Azoospermia – Causes, Diagnosis, and Treatment
Introduction
Did you know that about 1 in every 100 men faces a condition where no sperm is found in their semen? This condition is called azoospermia, and it is one of the leading causes of male infertility. Studies show that 10–15% of men struggling with infertility are diagnosed with azoospermia, making it a serious yet often overlooked concern. What makes it more challenging is that most men with azoospermia show no obvious symptoms; they only discover it when pregnancy doesn’t happen, even after a year of trying.
The good news? With the help of modern fertility treatments, men diagnosed with azoospermia still have a real chance to achieve biological fatherhood. At Imprimis IVF, modern treatments like micro-TESE, ICSI, and advanced genetic testing give couples real hope. Proper treatment and timely diagnosis mean azoospermia doesn’t have to stop someone from becoming a parent. It’s just the beginning of a new path.
Understanding Azoospermia
Azoospermia simply means that a man’s semen contains no measurable sperm. While it may sound rare, research shows it affects around 1% of all men worldwide and nearly 10–15% of infertile men. In India, some studies report even higher numbers due to factors like infections and untreated reproductive health issues.
There are two main types of azoospermia. In Obstructive Azoospermia (OA), the testicles make healthy sperm, but a blockage in the reproductive tract prevents them from reaching the semen. In Non-Obstructive Azoospermia (NOA), the problem lies in sperm production itself; either the testes produce very few sperm or none at all. Around 40% of patients have obstructive azoospermia, whereas about 60% have the non-obstructive type.
Understanding which type of person one has is critical because treatments differ. While blockages may be corrected surgically, NOA often needs advanced fertility techniques like micro-TESE and ICSI. With proper diagnosis, couples can make informed decisions and explore the best path to parenthood.
Common Causes of Azoospermia
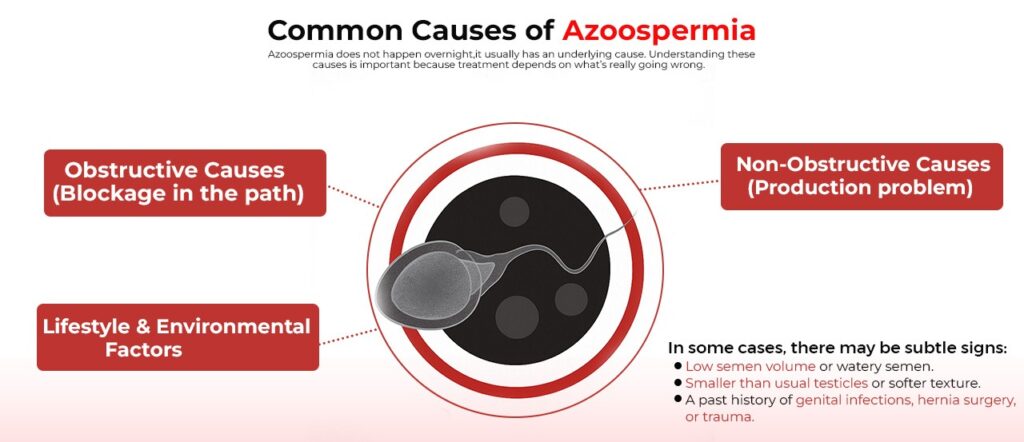
Azoospermia does not happen overnight; it usually has an underlying cause. Understanding these causes is important because treatment depends on what’s really going wrong.
Obstructive Causes (Blockage in the path):
Sometimes sperm are produced normally, but they cannot reach the semen due to a blockage. In India, infections like tuberculosis of the genital tract are a common reason for such blockages. Some men are born with a congenital absence of the vas deferens (the tube carrying sperm), often linked to CFTR gene mutations. Past surgeries, like vasectomy or hernia repair, may also cause obstruction. In older generations, even illnesses like smallpox led to scarring and blockages.
Non-Obstructive Causes (Production problem):
Here, the testicles themselves fail to make sperm. Genetic conditions like Klinefelter’s syndrome or Y-chromosome microdeletions are common culprits. Hormonal imbalances, such as very low levels of FSH, LH, or testosterone, can also affect sperm production. Testicular injuries, varicocele (swollen veins in the scrotum), or infections like mumps orchitis may damage fertility. In about 1 in 4 men, the cause remains unknown; this is called idiopathic azoospermia.
Lifestyle & Environmental Factors:
Modern lifestyles play a growing role. Smoking, alcohol, obesity, toxins, and stress can all reduce sperm health. Research indicates that infertility is increasing rapidly in urban parts of India, impacting nearly 10–15% of couples.
Symptoms & When to See a Doctor
What makes azoospermia unexpected is that it usually doesn’t present with clear symptoms. Many men with this condition have a completely normal sex life, normal erections, normal ejaculation, but discover the problem only when there is no pregnancy despite regular unprotected intercourse.
In some cases, there may be subtle signs:
- Low semen volume or watery semen.
- Smaller than usual testicles or softer texture.
- A history of genital infections, hernia surgery, or trauma.
According to global fertility guidelines, couples should seek medical evaluation if no pregnancy occurs after 12 months of regular, unprotected sex (after 6 months if the female partner is over 35). In India, infertility affects nearly 27.5 million couples, and male factors account for almost 40–50% of cases.
Azoospermia not only affects the body but also carries a deep emotional burden. Men often feel shocked, anxious, or even blame themselves. Early counselling and open discussions with fertility specialists help couples cope better and move toward solutions.
Diagnosis of Azoospermia

Getting the right diagnosis is the starting point of any treatment. Since azoospermia can be caused by either a blockage (obstructive) or problems in sperm production (non-obstructive), doctors follow a systematic process to find the root cause.
1. Semen Analysis (Gold Standard):
- The most important test, done at least twice to rule out temporary issues.
- In azoospermia, semen appears normal but shows zero sperm under the microscope.
- In India, studies suggest that nearly 1 in 10 infertile men may have azoospermia detected through semen analysis.
2. Hormonal Testing:
- Blood tests measure FSH, LH, and testosterone.
- High FSH usually indicates poor sperm production (NOA), while normal levels may suggest a blockage (OA).
3. Genetic Tests:
- Tests like Karyotyping, Y-chromosome microdeletion, and CFTR mutation analysis help detect hereditary causes.
- Research shows that 15–20% of NOA cases are linked to genetic factors.
4. Ultrasound & Imaging:
- Scrotal ultrasound and TRUS (transrectal ultrasound) help identify blockages, cysts, or missing vas deferens.
5. Testicular Biopsy or mTESE (Micro-TESE):
- A minor procedure to directly check if sperm are being produced inside the testicles.
- If sperm are found, they can be retrieved and used for IVF/ICSI.
Treatment for Azoospermia
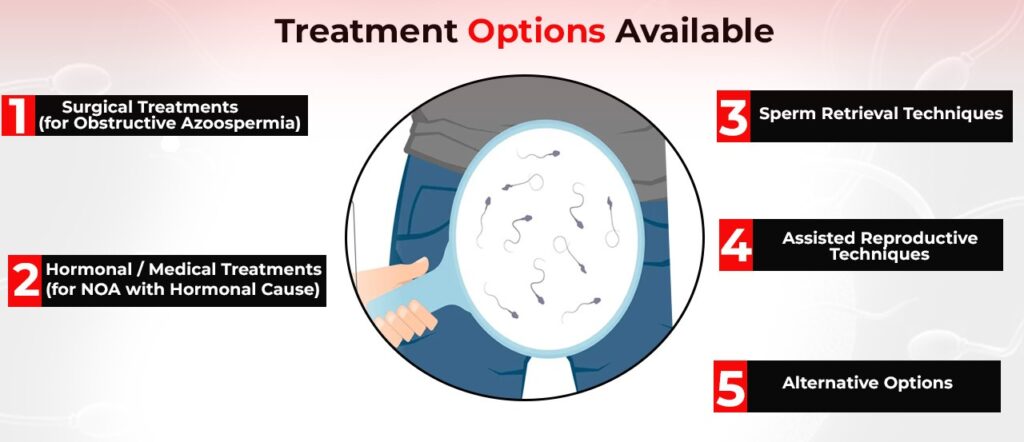
Azoospermia does not mean the end of fatherhood. Thanks to modern medicine, many men with this condition are now able to become biological fathers. Treatment depends on whether the cause is obstructive (sperm is made but blocked) or non-obstructive (sperm production problem).
1. Surgical Treatments (for Obstructive Azoospermia):
- If a blockage is the reason, microsurgical procedures like vasectomy reversal or reconstruction can restore the passage.
- TURED (Transurethral Resection of Ejaculatory Duct) is used for blockages in the ejaculatory ducts.
- Studies show that such surgeries can restore sperm in the semen in 50–70% of cases.
2. Hormonal / Medical Treatments (for NOA with Hormonal Cause):
- Some men with low hormones (FSH, LH, testosterone) benefit from hormone replacement therapy.
- Gonadotropin injections can stimulate sperm production in selected patients.
3. Sperm Retrieval Techniques:
When sperm is not seen in semen, doctors can directly retrieve it from the testicles or epididymis:
- PESA (Percutaneous Epididymis Sperm Aspiration)
- TESA (Testicular Sperm Aspiration)
- TESE (Testicular Sperm Extraction)
- Micro-TESE (Microsurgical Testicular Sperm Extraction) – the most advanced and successful, allowing retrieval in up to 40–60% of NOA cases.
Retrieved sperm can be frozen for later use in IVF/ICSI.
4. Assisted Reproductive Techniques (ART):
- With IVF + ICSI (Intracytoplasmic Sperm Injection), even a single healthy sperm is enough to fertilise an egg.
- In India, pregnancy rates through ICSI are around 40–55% per cycle, depending on age and clinic expertise.
- At Imprimis IVF, advanced embryology labs, time-lapse monitoring, and skilled embryologists maximise success for men.
5. Alternative Options:
- If no sperm can be retrieved, options like donor sperm or adoption can be considered. These choices are sensitive but help couples fulfil their dream of parenthood.
Latest Advances & Research
The treatment of azoospermia has seen remarkable progress in the past decade, giving hope to men who once had very limited options.
- Microdissection TESE (Micro-TESE):
Today, the gold standard for Non-Obstructive Azoospermia (NOA) is Micro-TESE. Using a high-powered microscope, doctors carefully identify tiny pockets of sperm inside the testis. Studies show that sperm retrieval rates can reach 40–60%, even in severe cases. - Genetic Screening:
Modern genetic tests, such as Y-chromosome microdeletion analysis and CFTR mutation testing help pinpoint the exact cause. This ensures the right treatment while preventing the risk of passing conditions to children. - Advanced Embryology Labs at Imprimis IVF:
At Imprimis IVF, cutting-edge labs with time-lapse imaging, microfluidics, and advanced culture systems increase fertilisation and embryo survival rates, bridging the gap between diagnosis and successful pregnancy. - Ongoing Research in India:
Leading institutes like AIIMS, PGI Chandigarh, and Kerala-based fertility centres are studying new techniques, including improved sperm retrieval and personalised hormonal therapy. - Future Scope:
Exciting fields like stem cell research and gene therapy are being explored worldwide. In simple terms, these could help the body “restart” sperm production in men with complete testicular failure, something once thought impossible.
Why Choose Imprimis IVF for Azoospermia Treatment?
When it comes to treating azoospermia, choosing the right centre makes all the difference. At Imprimis IVF, we bring together science, expertise, and compassion to help couples achieve parenthood.
- Specialised Expertise in Male Infertility:
Our doctors have years of focused experience in diagnosing and treating azoospermia, from simple blockages to complex genetic causes. - Advanced Diagnostics & Treatments:
We provide state-of-the-art genetic testing, hormonal evaluation, ultrasound, and Micro-TESE, the gold standard for sperm retrieval in non-obstructive cases. - High Success Rates with IVF/ICSI:
Even a single healthy sperm can lead to a healthy baby with ICSI. At Imprimis, our IVF success rates are among the highest in Eastern India,40–55% per cycle, comparable to top global standards. - Experienced Team & World-Class Labs:
Our embryologists use advanced tools like time-lapse imaging and modern incubators to ensure the best possible embryo development. - Personalised & Ethical Care:
We understand the emotional journey of infertility. From counselling to treatment, every step is tailored to your needs, with full transparency and ethical practices.
For couples facing azoospermia, Imprimis IVF is not just a clinic; it’s a trusted partner on the path to parenthood.
Conclusion
Azoospermia may sound overwhelming, but with the right diagnosis and modern treatments, fatherhood is very much possible. Advances like micro-TESE, ICSI, and genetic testing have transformed outcomes for men who once had no hope. At Imprimis IVF, couples receive not only world-class technology but also compassionate support at every step. With expert guidance, most men with azoospermia can still fulfil their dream of becoming fathers.

